The Commonwealth Fund approached its 20th presidential election in 2024 with a note of optimism. Although it has long known that much is not well with the American health-care system, it could point to recent improvements and reforms.
The New York and Washington DC-based foundation, which has been around for 107 years and is currently led by Joseph R. Betancourt, M.D., M.P.H, states its purpose is to "promote a high-performing health care system that achieves better access, improved quality, and greater efficiency, particularly for society's most vulnerable, including low-income people, the uninsured, and people of color."
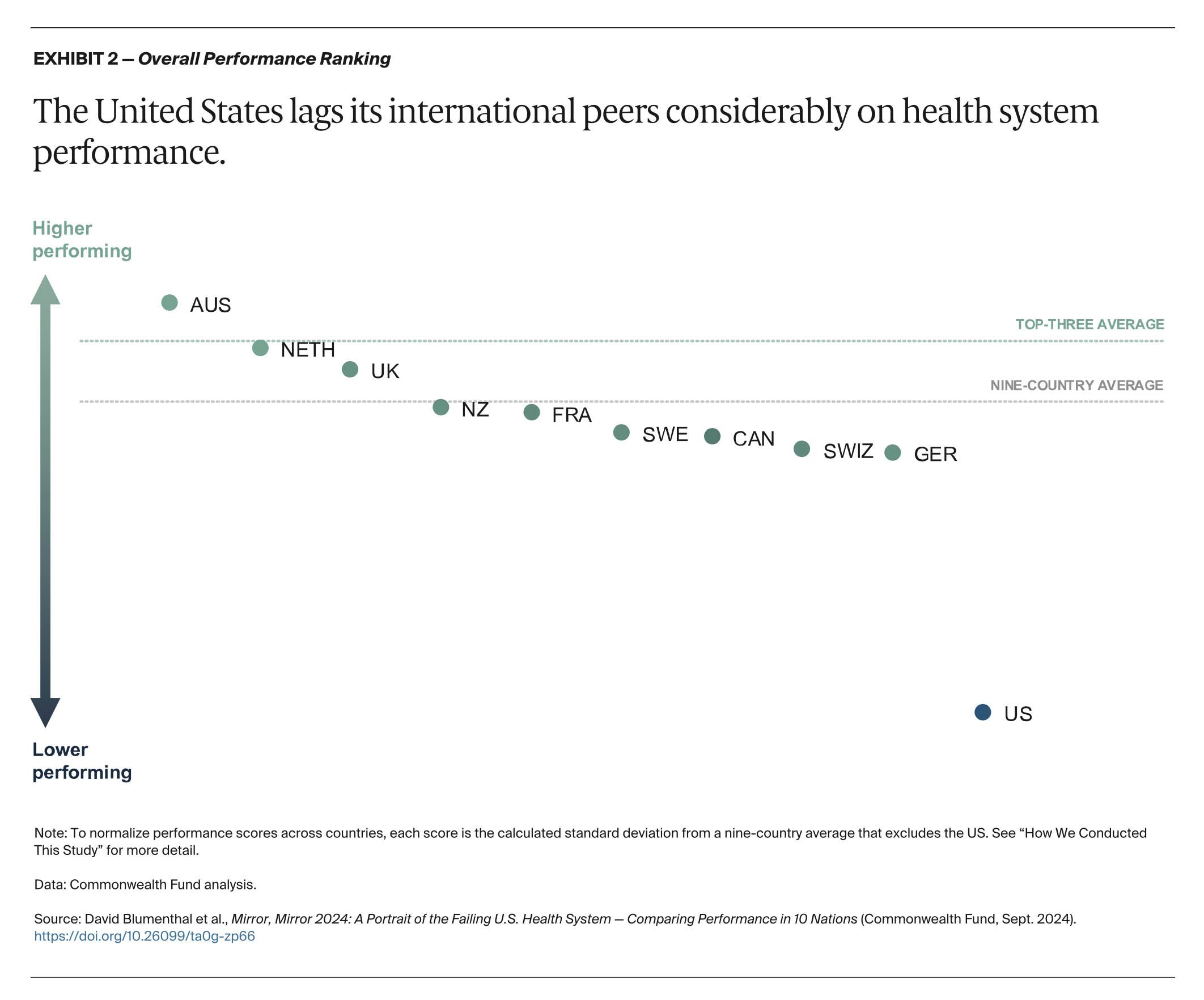
The Commonwealth Fund has published at a rate of every three years or so, since 2004, a report it calls “Mirror Mirror,” which looks at this country’s health-care system alongside several others. The 2024 edition compared the United States with nine other countries.
That most recent “Mirror Mirror,” the eighth, says, “The U.S. continues to be in a class by itself in the underperformance of its health care sector. While the other nine countries differ in the details of their systems and in their performance on domains, unlike the U.S., they all have found a way to meet their residents’ most basic health care needs, including universal coverage.”
This is all the more remarkable given that the U.S. spends more than 16 percent of its GDP on health care whereas in the other countries studied in the report the figure is between 8 percent and 12 percent.
One of the serious deficiencies of our health-care system is its relative weakness as a safety net, and the huge Medicaid cuts in the One Big Beautiful Bill Act are hardly going to help.
“Cuts of this magnitude are not going to discriminate based on whether you have Medicaid or not,” said Rachel Nuzum, Vice-President for Policy at the Commonwealth Fund, in a July 17 webinar reported on by the Echo.
“Mirror Mirror” 2024 analyzed Australia, Canada, France, Germany, the Netherlands, New Zealand, Sweden, Switzerland, the United Kingdom, and the United States. It did not include Norway, the best performing nation in the previous report, because it exited in 2022 the International Health Policy Survey, which is based on interviews with physicians and patients.
One goal in comparing systems is “to glean insights for U.S. improvement.” Underlying its method is an analysis of “70 health system performance measures” in five areas, which are: “access to care,” “care process,” “administrative efficiency,” “equity” and “health outcomes.”
Its most fundamental finding was, “The top three countries are Australia, the Netherlands, and the United Kingdom, although differences in overall performance between most countries are relatively small. The only clear outlier is the U.S., where health system performance is dramatically lower.”
Not only is the U.S. 10th of the 10 countries, it seriously lags behind in four of those five overall areas studied, whereas the other nine examined “are more alike than different with respect to their higher and lower performance in various domains.”
The report says, “Despite spending a lot on health care, the United States is not meeting one of the principal obligations of a nation: to protect the health and welfare of its residents. Most of the countries we compared are providing this protection, even though each can learn a good deal from its peers. The U.S., in failing this ultimate test of a successful nation, remains an outlier.”
The best news from an American perspective is that in one of the report’s five main areas, “care process,” it comes in second behind New Zealand, with Canada and the Netherlands close behind, while Sweden performs comparatively poorly.
The report explains, “Care process looks at whether the care that is delivered includes features and attributes that most experts around the world consider to be essential to high-quality care. The elements of this domain are prevention, safety, coordination, patient engagement, and sensitivity to patient preferences.”
It continues, “Strong U.S. performance in the care process domain is the result of the successful provision of preventive services, such as mammograms and flu vaccinations, and an emphasis on patient safety. With respect to preventive care, the U.S. record might reflect the vigorous pay-for-performance policies implemented by Medicare and other payers to reward the delivery of these services.
“A concerted focus in the U.S. on patient safety since the beginning of the century has yielded significant reductions in adverse events during hospital stays for heart attack, heart failure, pneumonia, and major surgeries between 2010 and 2019,” it adds.
“In the U.S.,” on the other hand, according to the Commonwealth Fund’s “Mirror Mirror” 2024 report, “lack of affordability is a pervasive problem. With a fragmented insurance system, a near majority of Americans receive their health coverage through their employer. While the ACA’s Medicaid expansions and subsidized private coverage have helped fill the gap, 26 million Americans are still uninsured, leaving them fully exposed to the cost drivers in the system. Cost has also fueled growth of private plan deductibles, leaving about a quarter of the working-age population underinsured. In other words, extensive cost-sharing requirements render many patients unable to visit a doctor when medical issues arise, causing them to skip medical tests, treatments, or follow-up visits, and avoid filling prescriptions or skip doses of their medications.”
It adds, “In terms of care availability, U.S. patients are more likely than their peers in most other countries to report they don’t have a regular doctor or place of care and face limited options for getting treatment after regular office hours. Shortages of primary care services add to these availability problems.”
In the July 17 webinar, the Commonwealth Fund’s Nuzum and two practicing doctors (Erin Emery-Tiburcio of Rush University Medical Center in Chicago and Harvard Medical School’s Sharon K. Inouye) attested to these problems and argued that the coming cuts will make them a good deal worse.
The 2024 edition of “Mirror Mirror” says, “Especially concerning is the U.S. record on health outcomes, particularly in relation to how much the U.S. spends on health care. The ability to keep people healthy is a critical indicator of a nation’s capacity to achieve equitable growth. In fulfilling this fundamental obligation, the U.S. continues to fail.”
For more information, go to commonwealthfund.org.