We hear the term “trickle-down” often. But “downstream” might be particularly apt for any discussion around the One Big Beautiful Bill Act. New York journalist Liz Seegert used the word when moderating a webinar* last Wednesday on that act’s consequences, both intended and unintended, as well as those unexpected by the population at large.
“A lot of people think it’s only the poor that are going to be affected by these changes,” said Prof. Sharon K. Inouye, Professor of Medicine at Harvard Medical School.
“Wrong. Wrong. Wrong,” Inouye declared during the webinar. “It’s going to be everyone. Middle-class, upper middle-class. It’s going to be all of us, and even the wealthy.
“If they have to go to the ER,” she said of the last-named category. “It’s going to be the same situation for them.”
The event entitled “Medicaid on the Chopping Block: How the Budget Bill Will Impact Older Adults” heard that the number of insured Americans could be reduced by 17 million, which would put the national figure at pre-Affordable Care Act levels. The triggering of significant job losses in the sector nationally was also discussed.
“Cuts of this magnitude are not going to discriminate based on whether you have Medicaid or not,” said Rachel Nuzum, Senior Vice-President for Policy at the Commonwealth Fund. “This is going to have major implications on provider burnout, willingness to engage, willingness to take insurance, willingness to take public programs, the ability for rural hospitals to stay open, the ability for community hospitals to stay open. Those are real and those issues don’t care who you get your coverage from.
“If the hospital is gone, the hospital is gone.
“It’s part of a whole suite of activities,” Nuzum added. “We can’t even look at this bill in isolation. We have executive orders starting in November; we see budget requests relating to HHS [Health and Human Services]; we see the rescission exercise happening right now.”
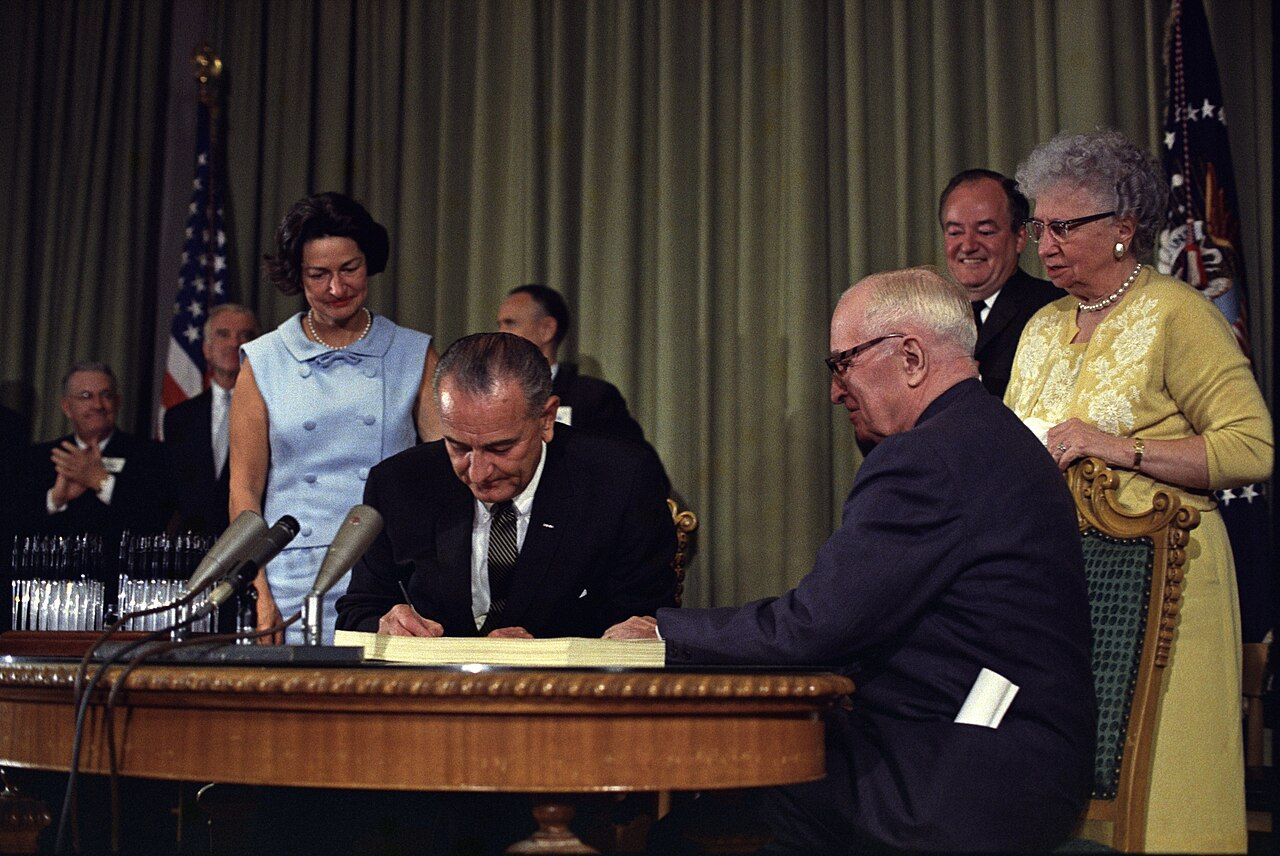
The panel’s experts spoke of the various ways that Medicaid and Medicare, both signed into law by President Johnson on July 30, 1965, are inextricably linked and overlap in practical ways.
Said Inouye, “Sixty-three percent of persons in nursing homes right now in our country are supported by Medicaid and that includes middle-class, upper middle-class, because nursing home care is so expensive.
“People won’t be staying in nursing homes, nursing homes are going to close and the anticipation is that there are about 500 nursing homes that are at immediate risk of closure.
“In a recent survey 25 percent of nursing home directors reported that they may have to close in the next 1-2 years with this degree of cuts.
“The nursing home where I work at, they’re very scared and they’re a model nursing home.”
Generally family members would prefer that elders would not have to go to a nursing home, but options for home care will also be hit; caregivers, both formal and informal, are disproportionately covered by Medicaid and many will almost certainly be joining the ranks of the uninsured.
The lowering of the numbers of people on Medicaid is an intended consequence of the OBBBA, as passed by the Senate.
“We are anticipating many more administrative hurdles,” Nuzum said.
There is particular concern about the work requirements, state by state, for the one in five Americans from age 50 to 64 who are on Medicaid. “Five million of those have Medicaid due to the Medicaid expansion that has been taken up by all but 10 states,” Nuzum said. “We know that this population is more likely to have a disability and/or chronic condition.”
Nuzum said that even in states that invested in IT and verification systems "the vast majority of people that lost coverage were people that were still eligible for the [Medicaid] program...they were kicked off for administrative reasons or failure to meet the administrative requirements."
She said in the past month she's heard people over the past liken the administrative burden to "asking someone to complete their taxes twice a year.
"People don’t have time,” she said, particularly if they're contending with chronic illnesses.
Nuzum referred to the “perfect storm” brewing in health-care provision, but particularly for older and poorer Americans. Dr. Erin Emery-Tiburcio agreed, saying professionals were already in 2025 facing “serious challenges.”
Said Emery-Tiburcio, who is Professor of Geriatric and Rehabilitation Psychology and Co-Director of the Center for Excellence in Aging at Rush University Medical Center in Chicago, “Over time we've had a declining number of geriatricians. By 2030, we're going to need 30,000 and right now we've barely got 7,000. So this is a long-standing challenge made worse by current cuts.”
Geriatricians are the lowest paid specialty, she explained, because of a variety of factors, with societal ageism at the top of the list, but issues around reimbursement being another.
Emery-Tiburcio said hospitals are already doing “more with less” and suffering “burnout,” but she’s also concerned about the emotional impact on patients. She cited one example, using a fictitious name, “Barbara is terrified she’s going to lose her Medicaid. She has a whole host of illnesses. And as such, she sees a primary care doctor. She goes to a whole bunch of specialists and she has a care manager in her primary care. Barbara is terrified that she is going to lose her Medicaid because if she has only straight Medicare, there are so many services she won't get.”
“It’s absolutely and overwhelming and scary right now,” Inouye said, adding that she is focused on the “direct impact that I’m anticipating for patients and families that I care for.”
Inouye added, “The reality is that many people will have to lose their jobs to take care of the elders in their families.
“It’s going to impact home-care. Those are things that we've seen in prior Medicaid cuts are the first thing to go unfortunately and so many of our home and community based services for the older population and these are the services that have been proven to keep people out of nursing homes. Unfortunately, those are going to go.
“I have many, many families that depend on these programs to help care for the elders in their family,” Dr. Inouye said, “[And] that’s going to be a huge burden on society and our communities as well.
“So we are losing a lot of the community and social safety net that we currently have in place,” she said. “It’s the fabric of our lives that holds all families together, those things are going to start to fray.
“ERs are already overloaded in all the Boston hospitals. Heaven forbid you have to go to a nursing home. The waits are unbelievable. Older adults are routinely boarded in a nursing home for days, sometimes weeks before they can get a hospital bed.”
Inouye added that being boarded in a nursing home “is associated with a high mortality rate because your standard care is not happening, your basic daily needs cannot be attended to, because you’re on a stretcher in the hallway for hours and days.
“Everyone is aware of it and yet we can’t change it,” she added. “So, it is a really, really, really discouraging time.”
People “of means” are seeing the “handwriting on the wall.”
Inouye said, “I’m already getting contacted on a daily basis by wealthy people saying, ‘Will you be my geriatrician?’ They want to hire me to be their personal geriatrician.
“I tell them ‘I’m sorry, no. I’m trying to figure out how to keep our systems alive here.’”
Dr. Inouye preferred to conclude her remarks on an optimistic note. “We have angels walking on this earth,” she said. “And so we will survive one way or the another. We may go back a century in our healthcare. But hopefully we will be able to keep things going. And I hope people will wake up and realize, and we will be able to change our policies and our priorities in this country and be able to rebuild our system after it's blown up, to improve efficiency and improve quality.
“You know after things are un-built, they can be rebuilt to be better. And more efficient and more equitable,” she said. “And so maybe we will have the opportunity to do that as we plan forward because we're learning.
“We're learning all these levels of how everything integrates with
everything else. And so we have the chance now to set it up better, to better integrate community care, preventive care with medical care.”
Dr. Inouye said, “I really do think if we get a reboot, we need to rethink our whole health care system, our whole community care system. They all need to be integrated and that will ultimately provide better care for the older population probably more efficiently and with less need for nursing homes. If we could provide better support to families, we can keep a lot of people out of nursing homes.”
* The webinar was part of a series by the Journalists in Aging Fellowship Program, an initiative of the Gerontological Society of America and Journalists Network on Generations. Almost 250 fellows have participated in the program, which welcomes applications for 2025, its 16th year, here.